The Future of Medical Clarity with Advanced AI Imaging

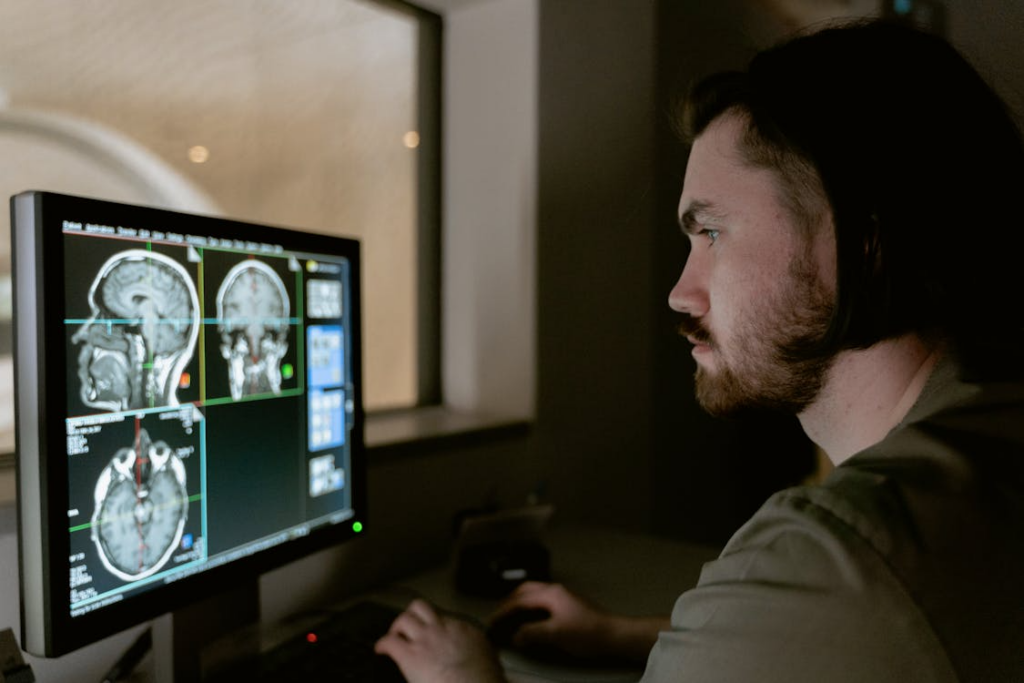
The landscape of modern medicine is shifting rapidly toward a digital-first approach that prioritizes precision and speed. We are currently witnessing a massive transformation in how doctors identify internal health issues. Advanced AI diagnostic medical imaging systems are at the heart of this technological revolution. These systems do more than just take pictures; they interpret complex biological data with incredible accuracy. By integrating machine learning into radiology, we can now detect diseases much earlier than ever before. This leap in technology is saving lives by providing a level of detail that the human eye might occasionally overlook. It is an exciting time to explore how these tools are reshaping patient outcomes and clinical workflows.
Understanding the Core of AI Imaging

Medical imaging has always been a cornerstone of effective diagnosis and treatment planning. Traditional methods like X-rays and MRIs have served us well for many decades. However, the sheer volume of data produced today can overwhelm even the most experienced specialists.
This is where artificial intelligence steps in to bridge the gap between data and insight. AI algorithms are trained on millions of existing medical images to recognize patterns. They can identify the smallest anomalies in tissue density or blood flow. This capability reduces the margin of error significantly in high-pressure hospital environments.
Radiologists use these tools to prioritize urgent cases that require immediate attention. The software acts as a second set of eyes that never gets tired or distracted. It can process hundreds of scans in the time it takes a human to review one. This efficiency is crucial for managing the growing backlog in global healthcare systems. Better imaging leads to better decisions and more personalized care for every patient.
Key Components of Modern Diagnostic Tools
A. Advanced Neural Networks for Pattern Recognition.
B. Automated Segmentation of Organs and Lesions.
C. Cloud-Based Platforms for Real-Time Data Sharing.
D. Deep Learning Models for Predictive Health Analysis.
E. Enhanced Image Reconstruction for Lower Radiation Doses.
F. Integrated Decision Support Systems for Clinicians.
The Evolution of Radiology Software
The journey of imaging software began with simple digital storage and basic viewing tools. Early systems were designed just to move away from physical film and chemicals. As computing power increased, so did the complexity of the analysis performed by the software. We moved from simple 2D images to highly detailed 3D reconstructions of the human body.
Modern tools now utilize “Deep Learning” to understand the context of an image. The software doesn’t just see pixels; it understands the anatomy it is looking at. It can differentiate between a benign cyst and a potentially malignant tumor. This distinction is vital for avoiding unnecessary biopsies and reducing patient anxiety.
Developers are focusing on making these tools more accessible and user-friendly. User interfaces are being designed to integrate seamlessly into existing hospital databases. This ensures that a doctor can access AI insights without leaving their primary workspace. Interoperability is the current gold standard for new medical imaging software.
Benefits of AI Implementation in Clinics
Implementing AI tools brings a variety of tangible benefits to medical facilities. The most obvious advantage is the drastic reduction in diagnostic turnaround time. Patients no longer have to wait weeks to hear back about their critical scan results. This speed allows for faster initiation of life-saving treatments like chemotherapy.
Furthermore, AI helps in standardizing the quality of care across different regions. A small rural clinic can access the same diagnostic power as a major urban hospital. The software compensates for differences in equipment quality or technician experience. It levels the playing field for patients regardless of their geographical location.
There is also a significant financial benefit for healthcare providers over time. Early detection often leads to less invasive and less expensive treatment options. By catching a condition in its infancy, the total cost of care is lowered. This makes healthcare more sustainable for both the provider and the patient.
Overcoming Challenges in AI Integration
Despite the benefits, integrating AI into the medical field is not without its hurdles. Data privacy is a major concern that developers must address with rigorous encryption. Patient records must be protected while still allowing the AI to learn from the data. Finding the balance between innovation and security is a continuous process.
There is also the challenge of “algorithmic bias” in some machine learning models. If the training data is not diverse, the AI might perform poorly on certain demographics. Engineers are working hard to ensure that datasets represent all ethnicities and ages. Diversity in data is essential for creating a truly universal diagnostic tool.
Finally, there is the human element of trust and professional adoption. Some practitioners may feel threatened by the idea of a machine “doing their job.” The goal is to frame AI as a collaborative partner rather than a replacement. Education and training are key to helping staff embrace these new digital colleagues.
The Role of Big Data in Imaging
Big data is the fuel that powers every advanced AI imaging system. Every scan performed contributes to a larger pool of knowledge that benefits everyone. By analyzing trends across large populations, AI can identify emerging health threats. This macro-level view is impossible for a single doctor to achieve on their own.
Predictive analytics allow doctors to foresee potential complications before they happen. If a patient’s scan matches a pattern of high risk, the system flags it immediately. This proactive approach moves medicine from reactive treatment to preventive care. It is a fundamental shift in how we perceive and manage human health.
Data security protocols are getting stronger to match the value of this information. Sophisticated layers of protection ensure that medical insights remain confidential. The future of medicine relies on our ability to manage this data ethically and efficiently.
Technical Capabilities of Modern Systems
A. Automated Detection of Small Lung Nodules.
B. Bone Age Assessment via Pediatric Radiographs.
C. Cardiac Functional Analysis for Heart Disease Detection.
D. Detection of Intracranial Hemorrhages in CT Scans.
E. Evaluation of Breast Density in Digital Mammography.
F. Fast Identification of Large Vessel Occlusions in Stroke Patients.
G. Grading of Prostate Cancer through Multiparametric MRI.
Enhancing Patient Experience and Safety
The patient experience is greatly improved when AI is part of the diagnostic process. One major safety improvement is the reduction of radiation exposure during scans. AI can “clean up” noisy images, allowing technicians to use lower doses of radiation.
This is especially important for children and patients who require frequent monitoring. Reduced wait times also lead to less stress and better mental health for patients. Knowing that a sophisticated system has verified their results provides peace of mind. Patients feel more confident in a diagnosis that has been double-checked by technology.
Transparency in how these tools work helps build trust between doctors and patients. AI can also help in explaining the results to the patient in a visual way. Color-coded maps and 3D models make it easier for a layperson to understand their condition. When a patient understands their health, they are more likely to follow treatment plans. This collaborative environment fosters better long-term health outcomes for everyone.
Looking Toward the Future of Healthcare
The future of AI imaging is moving toward even more specialized and localized tools. We may soon see portable imaging devices that use AI to diagnose patients in the field. Emergency responders could use these tools to assess trauma at the scene of an accident. This would bring hospital-level expertise to the very front lines of medical care.
We are also looking at the integration of AI imaging with other “omics” data. Combining imaging results with genetic info will create a complete biological profile. This “precision medicine” allows for treatments tailored to a person’s unique DNA.
The synergy between different tech fields will lead to breakthroughs we can’t yet imagine. Innovation in hardware will continue to complement the software advancements. Smaller, faster, and more sensitive sensors will provide even clearer data for the AI. The boundaries of what we can see inside the human body are constantly expanding. We are entering an era where no disease can remain hidden for long.
Final Thoughts on AI Integration
The adoption of AI in medical imaging is a journey of continuous improvement. It requires a partnership between engineers, doctors, and regulatory bodies. As the technology matures, it will become an invisible but essential part of every checkup. The ultimate goal is to make high-quality healthcare a standard for all people.
We must remain vigilant about ethical standards as we develop these powerful tools. The focus should always remain on the well-being of the individual patient. Technology is merely a vehicle to deliver more compassionate and effective care. The human touch in medicine will never be replaced, only enhanced by these systems.
As we look at the progress made, it is clear that the best is yet to come. Every update to an algorithm brings us closer to a world without diagnostic errors. The commitment to innovation ensures that medicine will keep pace with human needs.
Conclusion
The integration of artificial intelligence into medical imaging represents a monumental shift in healthcare history. This technology offers a level of precision that was previously considered impossible for human practitioners alone. By automating the most tedious aspects of image analysis, we allow doctors to focus on the human side of medicine. Early detection rates are climbing, which directly translates to more lives being saved every single day.
Patients benefit from reduced radiation exposure and faster results that lead to immediate action. The challenges of data privacy and algorithmic bias are being met with rigorous scientific and ethical standards. We are moving toward a future where diagnostic errors are becoming a relic of the past. Modern clinics that embrace these tools are setting a new standard for excellence in patient care.
The synergy between human expertise and machine intelligence is the ultimate formula for medical success. As these systems evolve, they will continue to unlock new mysteries of the human body and improve global health.



